Exploring the Complexities of Long-COVID Research
Written on
Chapter 1: Understanding Long-COVID
Long-COVID encompasses a range of symptoms that persist after the acute phase of a COVID-19 infection, yet its definition remains unclear. This ambiguity raises questions about how we can accurately diagnose and treat those affected.
This paragraph will result in an indented block of text, typically used for quoting other text.
Section 1.1: Personal Accounts of Long-COVID
A colleague of mine experienced symptoms consistent with long-COVID two years ago. She suffered from significant fatigue and brain fog, which left her unable to work for several months. Although she has improved, she still feels less energetic than before. At only 24 years old, this raises the question: could her condition truly be attributed to COVID-19?
Long-COVID is identified by the presence of symptoms lasting more than 12 weeks following a COVID-19 infection, provided these symptoms cannot be explained by other medical conditions. Common diagnostic questions include: “Did you experience any symptoms lasting three months or longer that you did not have before contracting COVID-19?”
However, this definition seems quite broad. Essentially, it suggests that any symptoms appearing after a COVID-19 infection can be classified as long-COVID, assuming no other medical explanations exist. For instance, if someone develops ongoing fatigue after being infected with the virus, they might be diagnosed with long-COVID.
This leads us to a logical fallacy known as post hoc, ergo propter hoc, which means "after this, therefore because of this." It implies that if symptom X occurs following event Y (COVID-19 or a vaccine), then Y must be the cause of X. This fallacy is often used to argue against vaccine safety.
Source: The Logic of Science
Before the COVID-19 pandemic, chronic fatigue was already a prevalent issue, affecting between 10% to 30% of the population. Interestingly, the same percentage of COVID-19 survivors is cited as developing long-COVID symptoms.
What were the established causes of fatigue before the pandemic? These include:
- Lifestyle Factors: Poor sleep, substance use, and stress.
- Pre-existing Conditions: Issues like adrenal insufficiency, anemia, anxiety disorders, cancer, diabetes, heart disease, and others.
- Unknown Origins: Conditions such as chronic fatigue syndrome (CFS) were also prevalent.
While infections like the Epstein-Barr virus have been linked to CFS, they are not the sole contributors. Changes in immune or hormonal systems may also play a role. Thus, even prior to COVID-19, many individuals experienced unexplained fatigue that could easily be misdiagnosed as long-COVID if the virus had been prevalent at that time.
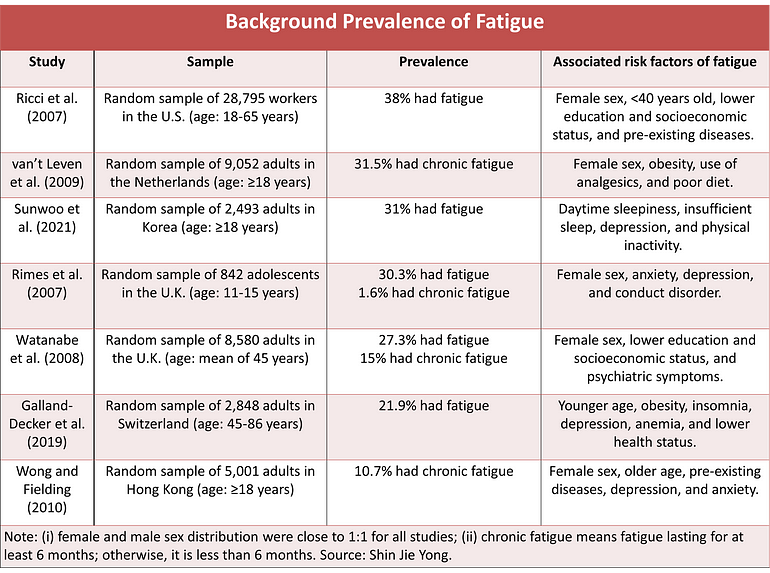
Figure 2. Rates of fatigue and chronic fatigue before the pandemic, sourced from various studies.
Section 1.2: Diagnostic Challenges
This brings us back to the question of certainty regarding my colleague's long-COVID diagnosis stemming from her COVID-19 experience. Unfortunately, we cannot claim complete certainty.
The ambiguity of long-COVID lies in its multifaceted nature; there is no singular mechanism that accounts for it. Consequently, there isn't a definitive test that can confirm a diagnosis of long-COVID. In contrast, identifying COVID-19 itself is straightforward: the disease is linked to the SARS-CoV-2 virus, which can be detected through RT-PCR testing.
I have authored several well-regarded studies on long-COVID, including one with a professor from the Public Health Agency of Canada. In our research, we identified six distinct subtypes of long-COVID based on underlying mechanisms:
- Multi-organ Sequelae (MOS): Some survivors display multiple organ-related symptoms detectable through imaging.
- Pulmonary Fibrosis Sequelae (PFS): Severe cases may develop lung scarring, especially in those who required mechanical ventilation.
- Chronic Fatigue Syndrome (CFS): Certain long-COVID patients may meet criteria for this condition.
- Postural Orthostatic Tachycardia Syndrome (POTS): This autonomic nervous system disorder can manifest in long-COVID patients.
- Post-intensive Care Syndrome (PICS): ICU survivors may experience long-term cognitive and physical effects.
- Medical or Clinical Sequelae (MCS): Existing conditions may worsen post-COVID.
There may well be additional subtypes, given the numerous proposed mechanisms of long-COVID, including viral persistence, immune dysfunction, and more.
Despite the diversity of these subtypes, current research often conflates them under the umbrella term "long-COVID." This amalgamation complicates our understanding of who is experiencing which specific symptoms.
This is not to imply that affected individuals are not ill; rather, we cannot definitively attribute their conditions to long-COVID resulting from previous infections. The assumption may be prevalent, but it can mislead us into oversimplifying a complex issue.
The challenge of treating long-COVID arises from this uncertainty. Should we consider antiviral treatments like Paxlovid for those with lingering symptoms? While testing for viral persistence could clarify this, the reality is that the virus might remain hidden in less accessible tissues, complicating matters further.
To effectively address long-COVID, we need to refine our understanding of its various forms—be it through subtypes, phenotypes, or endotypes—and identify biomarkers or imaging features that can clearly delineate long-COVID as a distinct condition.
If you’ve engaged with this content, thank you for your attention. You can subscribe to my Medium email list here. If you feel inclined, consider providing a tip; I would greatly appreciate your support.
Chapter 2: Video Insights on Long-COVID
This video, titled "Unlocking the Mysteries of Long COVID," delves into the nuances of long-COVID, exploring its diverse manifestations and the ongoing research efforts aimed at understanding this condition.
In the video "Update on Long Covid," experts share the latest findings and insights into long-COVID, shedding light on current treatment approaches and the implications for public health.